Since the 1980s, SSRIs and benzodiazepines have dominated the prescription medication scene for depression, anxiety, and panic disorder. SSRIs and benzodiazepines have largely replaced two older classes of medications: tricyclic antidepressants (TCAs) and the monoamine oxidase inhibitors (MAOIs).
There is also a miscellaneous or “atypical” group of antidepressants, simply because they do not technically fit into one of the other categories. The medications grouped in this category include buspirone (Buspar), mirtazapine (Remeron), trazodone (Desyrel), vilazodone (Viibrid), and vortioxetine (Trintellix).
All antidepressants work by modifying various chemicals in the brain, such as serotonin, norepinephrine, and dopamine. These chemicals all play different roles in mood, emotions, focus, motivation, and many other brain and body functions.
The term “antidepressant” gets misunderstood because it is not exclusively used to describe medicines that help depression. Antidepressants can also reduce anxiety and prevent panic attacks, among other uses. Every medication has officially approved uses by the Food and Drug Administration (FDA), and unofficial “off-label” uses. In the United States, physicians and other healthcare professionals are allowed to prescribe medications for reasons other than their FDA-approved uses.
Tricyclic Antidepressants
Tricyclic antidepressants, also known as TCAs, were first introduced in the late 1950s to treat depression. Their name describes their chemical structure. TCAs may be the right choice for some people who do not respond well to first-line medications. Some commonly prescribed TCAs (and their brand names) include:
- Amitriptyline (Elavil) – approved for depression; off-label for insomnia, anxiety, nerve pain, migraine prevention
- Clomipramine (Anafranil) – approved for obsessive-compulsive disorder (OCD); off-label for depression, anxiety, panic
- Desipramine (Norpramin) – approved for depression; off-label for anxiety, eating disorders, attention deficit hyperactivity disorder (ADHD)
- Doxepin (Sinequan) – approved for depression, anxiety, insomnia
- Imipramine (Tofranil) – approved for depression and bed-wetting; off-label for panic
TCAs work by increasing serotonin and norepinephrine levels, which can elevate mood and affect other brain chemicals. TCAs are effective, but their side effects make them less useful. The possible side effects include drowsiness, blurred vision, constipation, dizziness, dry mouth, blood pressure changes, sexual dysfunction, and weight gain or loss.
TCAs can worsen other conditions. TCAs are not recommended for people with vision problems such as glaucoma, or people with diabetes, heart arrhythmias, seizures, or liver disease. TCAs can also rarely contribute to serotonin syndrome, which can be life-threatening. Like all antidepressants, TCAs may increase suicide risk in children and young adults. Alcohol diminishes the antidepressant action of TCAs and may worsen side effects.
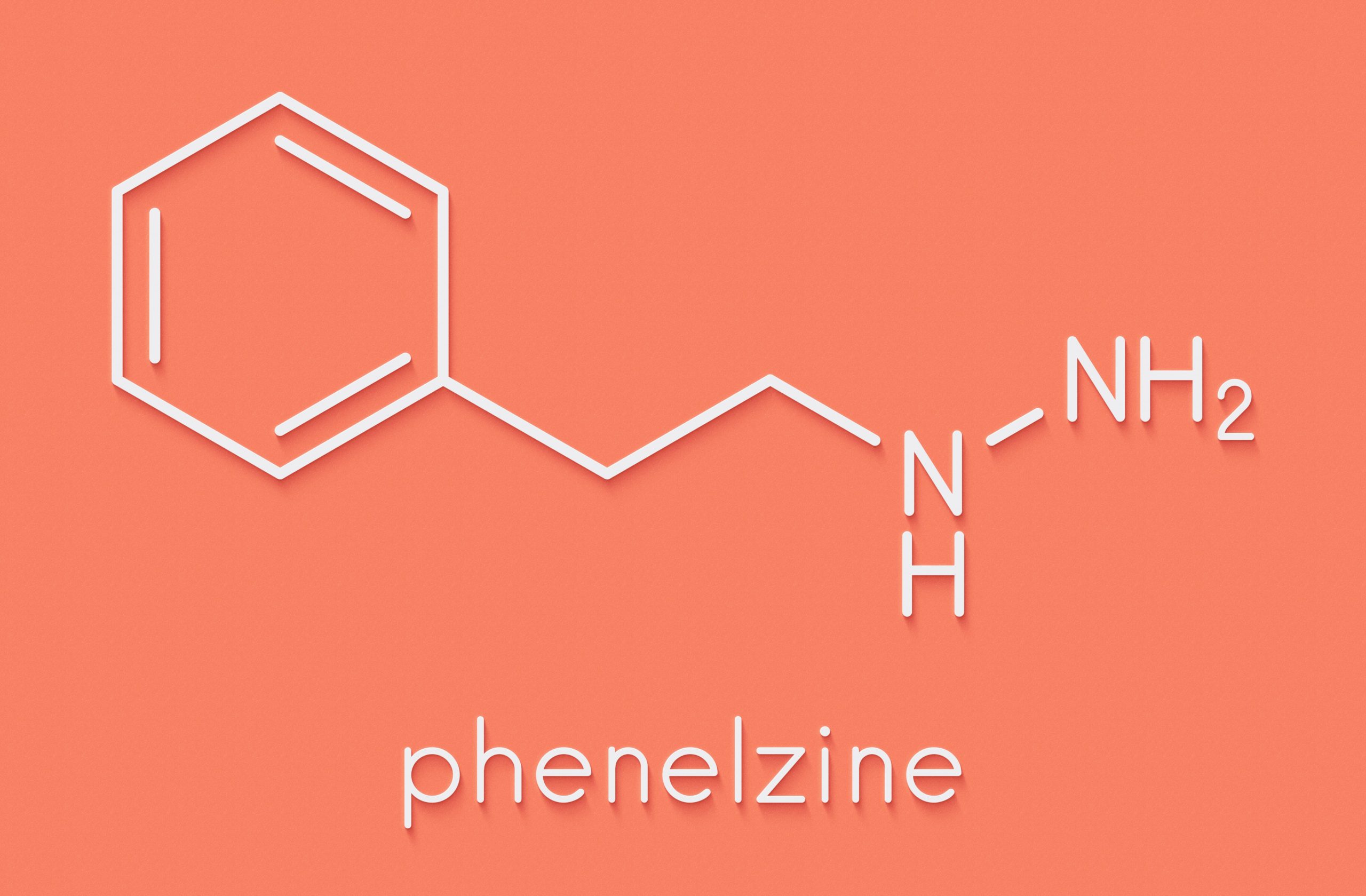
Monoamine Oxidase Inhibitors
Monoamine oxidase inhibitors (MAOIs) were the first-ever antidepressants and date back to the early 1950s. They block the enzyme that breaks down norepinephrine, serotonin, and dopamine. Today MAOI use for depression is limited to the last resort, only when all other treatment options have failed. Some MAOIs (and their brand names) include:
- Isocarboxazid (Marplan)
- Phenelzine (Nardil)
- Tranylcypromine (Parnate)
MAOIs can have dangerous reactions triggered by an extensive list of interacting medications, foods, and alcohol. Foods that contain tyramine can cause a sudden jump in blood pressure leading to confusion, seizures, coma, and death. Some examples of tyramine-containing foods are deli meats, aged cheeses, ripe fruits, fish, beer, and wine. No other antidepressants, pain medications, over-the-counter cold medicines, or any drugs should be taken with an MAOI without first checking with a doctor or pharmacist. Even after stopping MAOI therapy, these foods and medications should still be avoided for 14 days.
Even though MAOIs have fallen out of favor, some people can still benefit from them for the treatment of depression, panic, and phobias. Their doctors must go over the precautions and dietary restrictions before prescribing an MAOI. Individuals taking MAOIs should protect themselves by carrying identification cards or wearing a medic-alert bracelet.
“Miscellaneous” Medications for Anxiety and Depression
The “miscellaneous” or “atypical” group of antidepressants are each unique and do not belong to any other class. Atypical medications for anxiety and depression include:
- Bupropion (Wellbutrin)
- Buspirone (Buspar)
- Mirtazapine (Remeron)
- Trazodone (Desyrel)
- Vilazodone (Viibryd)
- Vortioxetine (Trintellix)
Bupropion (Wellbutrin) is FDA-approved for depression, seasonal affective disorder, and smoking cessation. Off-label, it is often prescribed for ADHD. Possible side effects are similar to SSRIs, except that, unlike most other antidepressants, bupropion does not cause weight gain or sexual problems. Extended-release forms of bupropion tend to have fewer side effects, including lower risk of seizures, a rare but severe side effect.
Buspirone (Buspar) is not an antidepressant and is in its own category of medication. Buspirone is an anxiolytic, or anxiety-relieving medication. Buspirone is primarily used to treat generalized anxiety disorder when first-line treatments (SSRIs, SNRIs, benzodiazepines) are not effective or cause intolerable side effects. Buspirone is generally well tolerated and has few side effects in most people and does not cause sexual side effects. Interestingly, if patients are responding to their SSRI treatment for their anxiety, but struggle with the potential sexual side effects, buspirone can be taken in addition to an SSRI to relieve sexual side effects. Buspirone is short-acting and must be taken 2 to 3 times per day. It is not useful for acutely subduing panic attacks because it takes 2 to 4 weeks to become effective.
Mirtazapine (Remeron) and trazodone (Desyrel) cause drowsiness and should be taken at bedtime. They are commonly prescribed for depression or anxiety in people that also have trouble sleeping. Side effects are similar to SSRIs, except heavier drowsiness, as mentioned.
Vilazodone (Viibryd) and vortioxetine (Trintellix), like SSRIs, block the reuptake of serotonin but also modify serotonin receptors in the brain. The FDA recently approved both for depression: vilazodone (Viibryd) in 2011 and vortioxetine (Trintellix) in 2013. Vilazodone (Viibryd) may cause insomnia and stomach upset and should be taken in the morning with food. Both of these newer medications seem to cause less weight gain and sexual problems compared to other antidepressants. Since both of these are relatively recent FDA approvals, they are not yet available as generic products and may be expensive. People may benefit from savings programs offered by the brand manufacturers of Viibryd and Trintellix.
Choosing the Right Medication
Several factors go into choosing the right medication for depression, anxiety, and panic disorders. Because many antidepressant medications are equally effective, the best medicine is the one that each individual can tolerate, with the fewest side effects. This is particularly true with weight gain and sexual side effects, which immensely impact a person’s health and quality of life. With dozens of options available, there is no reason to endure unpleasant side effects. Discussing side effects with a healthcare provider, while sometimes uncomfortable, is essential to exploring better options. With time, patience, and support, finding the right medication can be life-changing for those living with depression, anxiety, and panic disorders.